May 24, 2023
A Cosmopolitan Parasite: Tracking Toxoplasma Between Laboratory Diagnostics and Regionalized Public Health Measures
- 15:00 to 16:30
- Talk
- Practices of Validation in the Biomedical Sciences
- Hanna Lucia Worliczek
The intracellular protozoan parasite Toxoplasma gondii was described in 1908 but it took until the 1940s for it to be recognized as a human pathogen of substantial concern, and until the 1970s to unravel its full life cycle. This zoonotic agent can infect all mammals and birds and appears world-wide with a seroprevalence in human adults between ten and eighty percent in different countries. Consequently, Toxoplasma is often characterized as a cosmopolitan parasite. Yet, diagnostic, medical, and public health practices developed since the 1950s are by no means uniform on a global level and neither is its medical impact. Caused by transplacental transmission to the fetus following a primary infection of pregnant women, congenital toxoplasmosis can lead to abortions as well as to hydrocephalus or microcephalus, chorioretinitis, and intracerebral calcification in infants. Symptomatic acquired toxoplasmosis through non-congenital infection, on the other hand, was rare and in the late 1940s tissue cysts in organs were interpreted as signs of chronic asymptomatic infections – the most common form of toxoplasmosis in adults. In the 1970s however, reactivated chronic toxoplasmosis in immunocompromised patients was recognized as a fatal disease if left untreated, with a stark increase of cases in the onset of the HIV/AIDS epidemic in the early 1980s.
The diagnosis of toxoplasmosis in immunocompetent individuals heavily relies on serology. The Sabin-Feldmann dye test from 1948 was the first laboratory test considered reliable. It was complicated to perform and interpret but nevertheless remained a gold standard in Toxoplasma-serology for decades. Starting in the 1950s, alternative tests were consecutively introduced. Each new test stimulated debates about their accuracy and applicability among parasitologists, laboratory professionals, and pediatricians. With the introduction of compulsory national screening programs for congenital toxoplasmosis in Austria (1975), France (1978), and the GDR (1978) new actors got involved, including public health representatives, higher civil servants, and politicians. In parallel, screening of a large population posed new challenges to toxoplasmosis serology. This new situation enforced questions about the validity of each test along different realms of validity, including its diagnostic target, standardization, the accuracy of large-scale application, or the interpretation and implication of results. With the preparation and introduction of screening programs such questions left the realm of academic discourses and met with political agendas and administrative demands. Biomedical experts not only had to translate complex academic debates lacking unambiguous consensus but they also acted as lobbyists for diagnostic, treatment, and prevention strategies.
By taking questions about the validity of laboratory diagnosis of toxoplasmosis as a heuristic trajectory, the inclusion of toxoplasmosis-testing into the Austrian “Mutter-Kind-Pass,” a mandatory national screening program for pregnant women and children introduced in 1974, we gain access to cycles of validation and refinement of diagnostic tests and their reappearing negotiations between basic research, the clinic, and the political-administrative sphere. Moreover, these processes offer insights into the regionalized enactment of disease prevention and management, in part based on de-facto-differences, in part nourished by regional histories of knowledge production and once established public health traditions, always confronted with the prevention paradox.
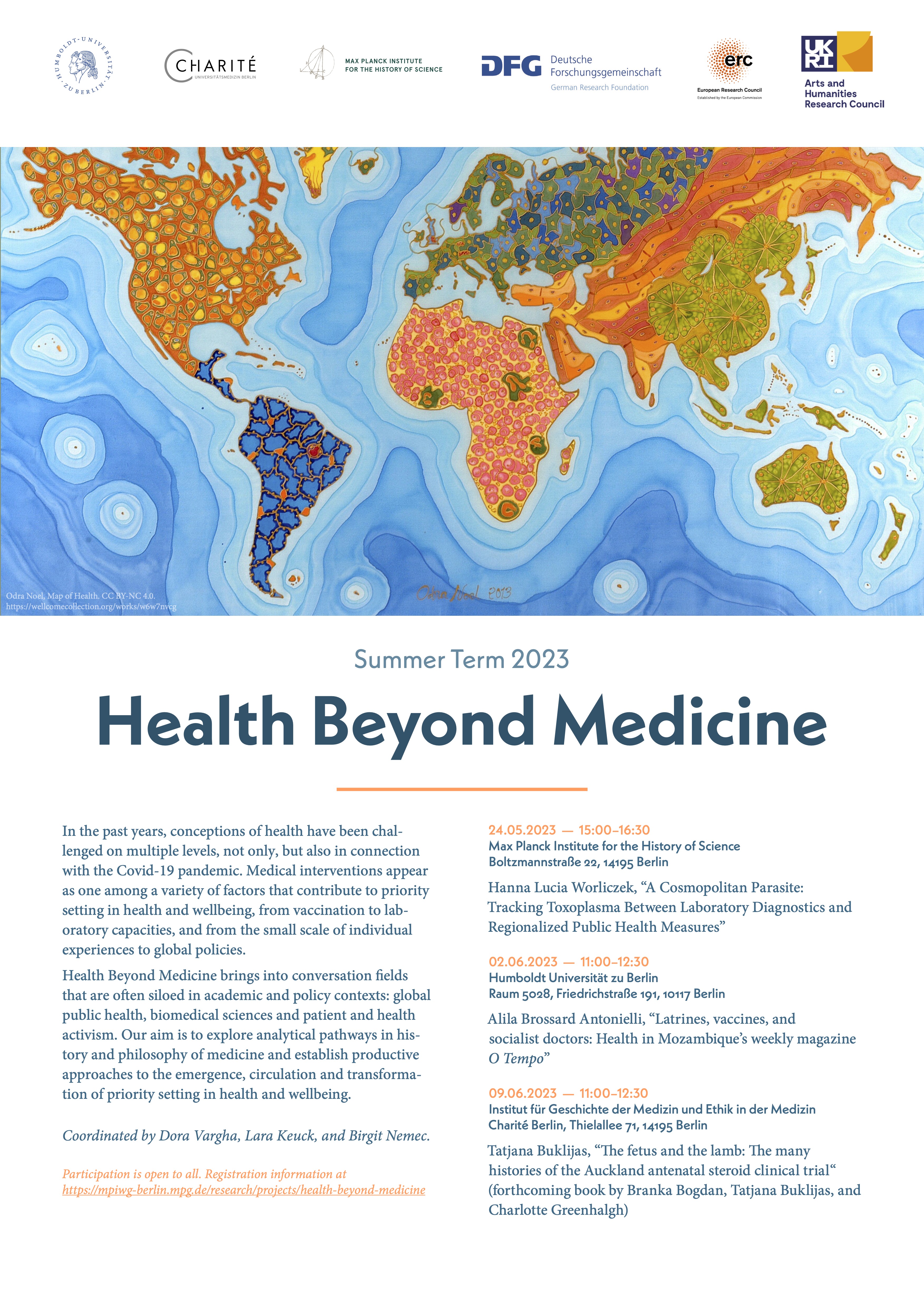
Contact and Registration
Participation is open to all. Please register by sending an email to Birgitta v. Mallinckrodt (officekeuck@mpiwg-berlin.mpg.de).